What is this disease with a convoluted name - hip disease? This disease is hip deforming joint disease, also commonly known as hip osteoarthritis.
Hip disease is currently the leading group of diseases of the musculoskeletal system, which are degenerative dystrophic in nature. There are many causes of hip arthropathy, and related to this, the disease is prevalent in all age groups.
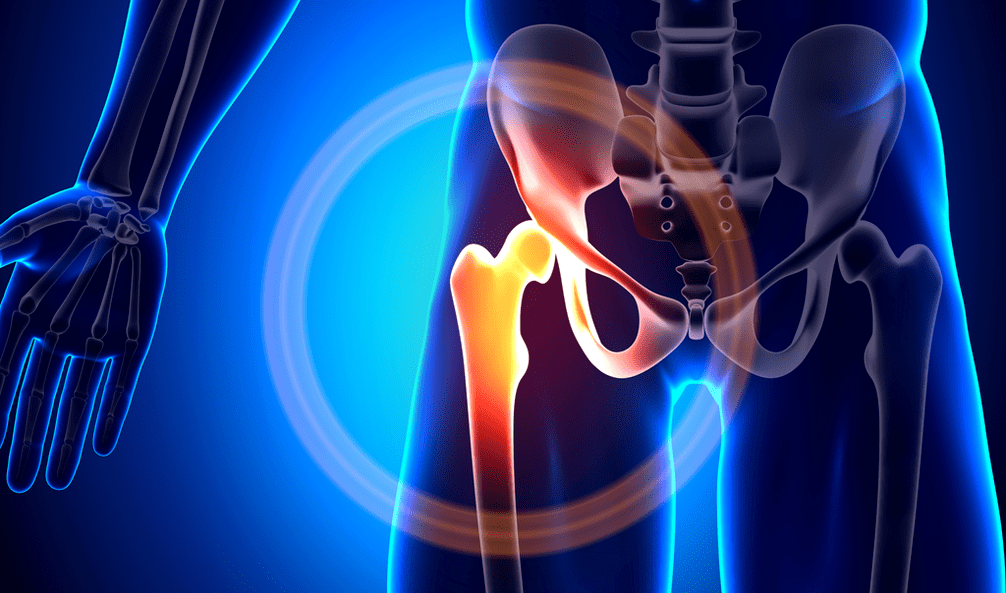
Hip arthropathy refers to a non-inflammatory arthropathy in which at first changes of the degenerative dystrophic nature of the cartilage of the hip joint, which line the surface of the articular bone, and in later stages the bone changes have occurred directly. Thus, during the progressive development of hip arthropathy, the natural normal function of the affected hip joint is violated, eventually leading to a violation of the function of the patient's musculoskeletal system, such as the entirety.
In most cases, hip joint disease affects people over the age of 40. Of course, hip disease, like any other disease, can be successfully treated without surgery, but only in the early stages. But in its later stages it is almost impossible without surgical intervention and only one thing can help avoid disability - joint prostheses affected by hip arthropathy. Unfortunately, people with hip disease don't value the mild pain of the hip joint in the early stages of the disease and avoid seeing a doctor, while hip osteoarthritis continues to develop day after day, gradually becoming more advanced forms.
How does hip disease develop?
Let's take a look at the mechanism of development of the disease hip arthropathy. Let's start with the fact that the hip joint consists of two bones:
- The end of the femur itself, which resembles a ball;
- The acetabulum, which resembles a small billiards bag, is located in the iliac part of the pelvis;
- Specialized articular cartilage on the surface of the two bones, similar to a spongy substance, necessary for shock absorbers, compressing when in motion and straightening when not;
- As well as the ligaments that form the hip joint cavity itself and thus the joint capsule.
In addition, there are musculature around the joints, such as the femur, gluteal muscles, etc. The condition of the hip joint also depends on its function.
During movement, when the articular cartilage is compressed, a specific fluid is "squeezed out" into the joint, which acts as a lubricant for the articular bones in the joint. In addition, the articular cartilage itself has the function of evenly distributing the load on the joint surface and is an excellent shock absorber during exercise.
The occurrence of hip joint disease is mainly due to the disturbance of the nutrition of the hip cartilage. The cartilage thins and then disappears in places. If nothing is done to stop this process, where the aforementioned cartilage atrophies, the bone itself grows directly, trying to "fill" the void created in the joint cavity. So, as a result of this skeletal change, osteophytes, which are "spikes" on the bone, begin to appear. These deformities, in turn, lead to disruption of the consistency of the articular bones in the hip joint, resulting in "wear and tear" of the remaining healthy areas of articular cartilage.
Causes of hip osteoarthritis
Causes of developing hip arthropathy can be classified as primary, of unknown etiology, secondary, due to other diseases such as, for example:
- Dislocation of the hip, which is congenital;
- hip dysplasia;
- aseptic necrosis of the femoral head itself;
- have suffered various previous injuries, such as a fractured femoral neck;
- Perth disease;
- Inflammatory processes of the hip joint;
Since hip arthropathy occurs not only in one hip, but also in both hips, it is quite possible to assert that bilateral hip arthropathy is not uncommon. Oftentimes, the knee or spine is affected, despite primary hip disease.
Symptoms of hip disease
The initial symptoms of hip joint disease directly depend on the degree of damage to the hip joint, as well as the stage of development of the disease, mainly:
- Pain that manifests in the hip joint during exercise and disappears at rest;
- appear lame;
- Stiffness of the hip joint;
- Downward progression of hip range of motion;
- Femoral muscle weakness and marked reduction in volume.
Additionally, we consider the symptoms of hip joint disease, depending on the extent of the disease:
- Symptoms of 1st degree hip disease: Moderate pain in the hip joint, which occurs only after a high load on the joint for a long time. After unloading and resting, the syndrome stops completely. For first-degree symptoms of hip arthropathy, the gait remained normal and the range of motion of the joints did not change.
- Symptoms of Degree 2 Hip Disease: The pains of the hip joint are already more intense than the first degree, and they also project into the groin area. Given the muscle wasting, the knee also started to hurt, and it was often more painful than the iliofemoral joint itself. Sometimes, with symptoms of secondary hip arthropathy, pain begins to appear even at rest, and after the load has been transferred to the affected joint, it has taken a considerable period of rest to relieve. Limping begins when running or walking for long periods of time. At the same time, the strength of the thigh muscles is considerably weakened and the range of motion of the joints is underestimated.
- Symptoms of third-degree hip disease: Persistent pain in the hip joint that does not go away even at night even after extremely long or continuous rest. The pain has affected the entire leg. In the context of pain, patients experience insomnia and various sleep disturbances. The muscles of the thighs, buttocks, and calves have strong atrophy, and the movement of the joints is almost minimal. When walking, patients are forced to resort to assistive devices, such as crutches, in order to get around.
If this hip arthropathy develops in the hip joint of only one leg, its weakened femoral muscle promotes the development of lateral displacement of the pelvis, with the result that the length and joints of the legs are affected and the hip arthropathy decreases.
Diagnosis of hip joint disease
When diagnosing hip arthropathy, the above symptoms of hip arthropathy must be considered in conjunction with data obtained from the patient's X-ray. This technique offers an opportunity not only to determine the extent of hip arthropathy, but also to identify the cause of the catalysts that lead to the development of hip arthropathy. Radiographs provide an excellent opportunity to identify changes that specifically lead to hip injury, which are directly related to the mechanisms by which hip arthropathy develops.
In addition to the diagnostic methods already listed, computed tomography and magnetic resonance imaging methods are also available, providing the opportunity to study in detail developing pathologies, such as the structure of bone tissue, the deformation of which is a concomitant of the disease. With regard to magnetic resonance imaging, this method can still assess the pathological disturbances experienced by the soft tissue surrounding the joints affected by hip arthropathy.
Treatment of hip joint disease
Treatment options for hip disease depend directly on the symptoms of hip disease and its stage. Typically, for first- and second-degree hip arthropathy, traditional conservative medical therapy is administered, including chondroprotective agents, vasodilators, and, if needed, muscle relaxants. NSAIDs are also used during particularly severe periods of hip disease. It should be remembered that this treatment must be carried out by a specialist because, unlike traditional medicine, self-medication has an extremely negative effect on the internal organs of the patient and completely inhibits the ability to restore the hyaline cartilage.

In addition, in the case of hip arthropathy, various physiotherapy procedures and exercise therapy are prescribed. Particularly effective in combination with traditional arthropathy drug treatment is the use of magnetic therapy in arthropathy treatment using special devices.
The impact of diet on the body of a person with hip disease has no direct therapeutic effect, but weight loss is recommended for obese individuals as it reduces the load on the affected joints, thereby reducing the acute symptoms of hip disease.
With grade 3 hip disease, the symptoms are the most painful, so it can only be treated with surgery, such as hip replacement. Statistics show that 95% of patients with hip osteoarthritis can fully restore the function of their limbs after surgery, allowing them to lead a fairly active lifestyle afterwards.
This prosthesis has a lifespan of about 15-20 years, but at the end of its useful life, a second surgery is required to replace the worn endoprosthesis.
notes,This is important! Do not diagnose yourself!If you have symptoms of hip joint disease, you should consult an orthopaedic doctor, as only a qualified specialist can make a correct diagnosis and prescribe the best treatment.
Prevent hip disease
Hip disease can be avoided if necessary precautions are taken:
- Mandatory and timely treatment of inflammatory joint diseases;
- Prompt treatment of joint dysplasia;
- Mandatory correct and reasonable physical activity, especially weight lifting, which must be performed correctly;
- Mandatory weight control to keep it normal;
- Prevent joint damage.































